Learn more about Anal Fistula
Dr Morris has a special interest in anal fistulas, and has published research and presented at conferences on the “Modern Management of Anal Fistulas”.
Anal fistulas are not a modern problem – and have existed since the days of Hippocrates – and likely even before this!
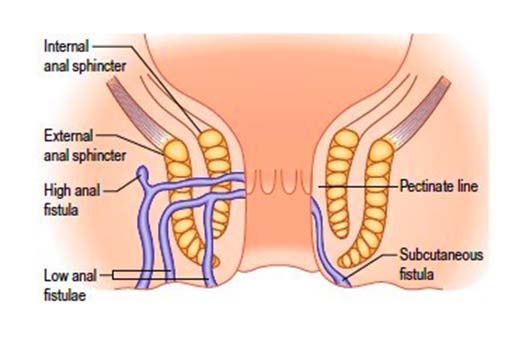
An anal fistula is an abnormal passageway from inside the anal canal to the skin of the buttock. This passageway occurs as the consequence of an infection, and often persists after an anal abscess is drained.
A fistula will act like a wound that doesn’t heal, close to the anus or on the buttocks. It may intermittently swell, become painful or tender, and discharge blood or pus, or both. It can leak and discharge fluid, and occasionally gas will pass down the fistula track. Unfortunately antibiotics won’t fix this problem, and it requires surgical assessment and intervention.
Please don’t be embarassed about anal fistulas – they are extremely common, and Dr Morris treats these every week. A fistula is NOT a reflection of poor hygiene. The application of soaps and excessive cleaning will not help the problem, and may cause further harms to the skin. There are no tablets, antibiotics, or over the counter creams or lotions that will heal an anal fistula.
There is no “one size fits all” operation for anal fistulas, and your colorectal surgeon must have a variety of techniques available to suit you and your particular history, your particular fistula, and your particular treatment goals.
The repair of a fistula can be challenging – and fistulas have always been challenging in surgical history! Fistula treatment can be challenging, as it is important to protect and preserve your normal sphincter muscle function (those muscles which allow you to control your bowel motions and wind).
Treatment options for the fistula depend on the type of fistula, the position of the fistula, and importantly – the degreeand any risks the patient has of incontinence. This includes possible injuries incurred at childbirth, with other diseases such as inflammatory bowel disease, radiation or cancer treatment, or previous anal or rectal surgery.
A ‘simple’ fistula is fortunately the most common type. A simple fistula is one that has a short and shallow passageway, , involves only a small amount of sphincter muscle, and in a patient without extra risks for incontinence. A simple fistula is treated most often by a ‘fistulotomy’, or a cut down onto the track to open it up. The wound is then allowed to heal without special packing or dressing.
A ‘complex’ fistula is more challenging for both the colorectal surgeon and the patient. A complex fistula may involve a significant amount of anal sphincter muscle, have multiple tracks, or occur in a patient who already has an increased risk of incontinence. These risks may include a history of a tear with childbirth, Crohn’s disease, or a history of radiation treatment.
A complex fistula may require additional workup – and sometimes your colorectal surgeon may use an ultrasound or MRI to help confirm clinical findings. A complex fistula requires a very clear understanding of what may be possible. Please read some of Dr Morris’ treatment principles below.
The first step in fistula management is to define the nature and the anatomy of the fistula. This is done definitively in the operating theatre, under a general anaesthetic. As will be discussed in the consultation, treatment proceeds at the same time depending on the findings.
A fistulotomy is ideally performed, but only if it is safe to do so, such as in a simple fistula.
If a fistulotomy is not considered safe, such as in a complex fistula, then inital management is often the insertion of a ‘draining seton’, a thin plastic cord (like a rubber earring for the anus) which helps allow any infection to resolve. This is usually a temporary measure and allows control of the fistula, and for things to ‘settle down’. Further surgery will be required to achieve a repair. Some patients may choose or need to have a seton permanently.
Operations that preserve muscle function need to be tailored to an individual patients specific circumstances, and your colorectal surgeon will discuss the possible treatments. Possible options include an anal fistula plug, fistula clip, ligation of intersphincteric fistula tract (LIFT), a rectal advancement flap (MAF/ERAF) and more. Each of these operations carry particularly reasons for, and against –
Dr Morris has a special interest in anal fistulas. In your consultation about your fistula, you will receive a simple explanation of the problem, and the commencement of an individualised strategy to work to achieve healing with minimisation of risks.
